Fertility preservation
Ovaries together with immature eggs develop early during fetal development before birth. Therefore, a newborn girl has already a stock of immature eggs in her ovaries. These eggs remain immature until she reaches puberty when the body’s hormonal system becomes active and stimulates maturation of eggs. Consequently, puberty is an important factor when fertility preservation is planned. If the patient has undergone puberty, the possibility to collect mature eggs to preserve fertility should be considered. If the patient has not gone through puberty, there are no mature eggs available, and the only option to preserve fertility is to collect and cryopreserve a piece of ovarian tissue that contains immature eggs.
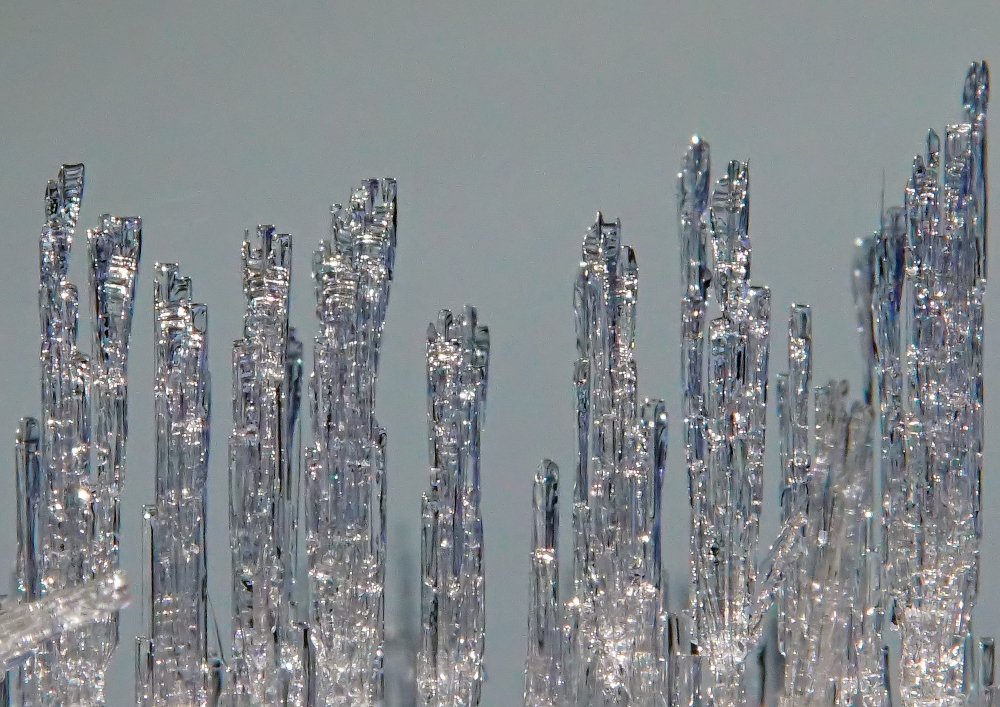
Sometimes ovarian tissue is collected for fertility preservation in adult women too. For example, if cancer treatments must be started immediately, ovarian tissue collection is the only procedure that can be performed rapidly because collection of mature eggs takes several weeks. A piece of ovarian tissue is surgically removed and stored in -180 °C. When the woman has recovered from cancer and wishes for pregnancy, the frozen ovarian tissue can be thawed and transplanted back. There are over 130 babies born after ovarian tissue transplantation in the world. The method is now considered established clinical routine for adult women. However, information on the suitability of this procedure for young girls is limited. There are only two known cases where ovarian tissue collected from girls have led to pregnancies after transplantation. In these cases, the girls were around 10 years old when the ovarian tissue was removed. We do not know if the method works for even younger patients. Importantly, tissue transplantation is not an option for all patients because the tissue may contain cancer cells that could return to the patient. This is the case for blood cancers like leukemias and lymphomas. For these patients, maturation of eggs in the laboratory could be an option in the future. However, no such method exists today.

Updated by:
andreasjonsson 2021-03-25